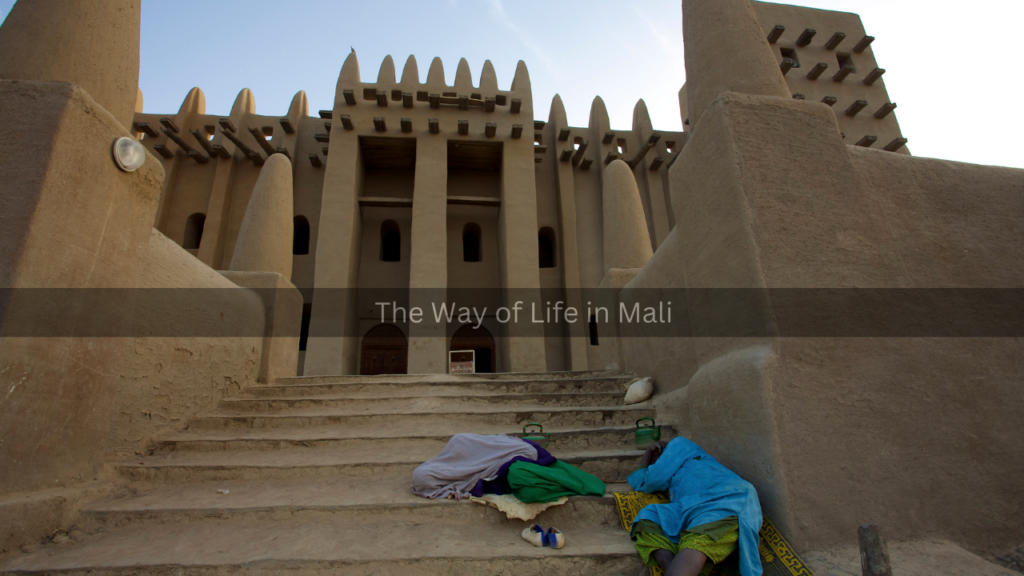
Mali, a landlocked West African nation, faces significant challenges in delivering adequate healthcare services to its population. With a largely rural population and a high burden of disease, the country struggles with limited medical infrastructure, insufficient healthcare professionals, and financial constraints. Despite these challenges, Mali has made notable progress in public health through innovative solutions and collaborative efforts with international partners.
Challenges in Mali’s Healthcare System
Mali’s healthcare system is hindered by several critical issues, including limited access to medical facilities, a shortage of healthcare professionals, and high rates of infectious diseases. The country’s vast geography and underdeveloped infrastructure make it difficult for rural populations to access medical care. Many communities rely on traditional healers due to the absence of nearby clinics or hospitals.
Another significant challenge is the shortage of trained healthcare professionals. The ratio of doctors to patients remains low, forcing many individuals to seek medical assistance from underqualified practitioners. Additionally, brain drain is a persistent issue, as many trained professionals migrate to other countries in search of better opportunities.
Mali also struggles with high rates of infectious diseases such as malaria, tuberculosis, and HIV/AIDS. Malaria remains one of the leading causes of death, particularly among children. Poor sanitation, lack of clean drinking water, and inadequate healthcare facilities contribute to the prevalence of these diseases.
Innovations and Progress in Public Health
Despite these challenges, Mali has implemented several innovative strategies to improve public health. One of the most successful initiatives is the expansion of community health programs. Community Health Workers (CHWs) play a crucial role in providing essential healthcare services, especially in remote areas. These workers are trained to offer basic medical care, administer vaccines, and educate communities about hygiene and disease prevention.
Vaccination programs have also been instrumental in reducing child mortality rates. Mali has partnered with global health organizations to increase immunization coverage, particularly for diseases like polio, measles, and meningitis. The success of these programs has contributed to a decline in child mortality over the past two decades.
Telemedicine has emerged as another promising innovation in Mali’s healthcare system. With the increasing use of mobile technology, healthcare providers can now consult with patients in remote areas, reducing the need for long-distance travel. This approach has been particularly beneficial for maternal and child healthcare, allowing pregnant women to receive medical advice and support without leaving their communities.
The Future of Mali’s Healthcare System
While Mali has made strides in improving healthcare, continued investment and international cooperation are crucial for sustained progress. Strengthening healthcare infrastructure, training more medical professionals, and increasing funding for public health initiatives will be key to overcoming the existing challenges.
Moreover, integrating traditional medicine with modern healthcare practices could enhance accessibility and cultural acceptance of medical treatments. By embracing a holistic approach and leveraging technological advancements, Mali can build a more resilient healthcare system that meets the needs of its growing population.
In conclusion, Mali’s healthcare system faces significant hurdles, but through community engagement, technological innovation, and strategic partnerships, the country is making progress in public health. Continued efforts to address these challenges will be essential in ensuring a healthier future for all Malians.